Flu Vaccinations Revisited
 Influenza season is coming, and with it, the latest recommendations for vaccinations. I have been reluctant to recommend them in the past. As a minimalist regarding pharmaceutical interventions, I like to see clear benefits that cannot be achieved through other means. My concerns have mostly to do with the effectiveness of the vaccines; numerous studies have questioned how well they work in practice. Also, because of frequent mutations, this is not the type of disease that is likely to be eliminated by vaccinations. Their usefulness, in my mind, would best be demonstrated by the reduction in related deaths. But while flu-related mortalities decreased dramatically over the last century, much of that decrease occurred before vaccination was common. The positive trend seems more likely related to improvements in life-saving medical care and overall health and poverty levels, etc.
Influenza season is coming, and with it, the latest recommendations for vaccinations. I have been reluctant to recommend them in the past. As a minimalist regarding pharmaceutical interventions, I like to see clear benefits that cannot be achieved through other means. My concerns have mostly to do with the effectiveness of the vaccines; numerous studies have questioned how well they work in practice. Also, because of frequent mutations, this is not the type of disease that is likely to be eliminated by vaccinations. Their usefulness, in my mind, would best be demonstrated by the reduction in related deaths. But while flu-related mortalities decreased dramatically over the last century, much of that decrease occurred before vaccination was common. The positive trend seems more likely related to improvements in life-saving medical care and overall health and poverty levels, etc.
However, there is some interesting evidence that we are going about vaccinations in the wrong way. If so, much better results might be obtained by taking a different tack. In general, the policy in the U.S., supported by the Centers for Disease Control (CDC), is to vaccinate those who are most at risk for serious illness or death. For influenza, this has meant the youngest and the oldest populations. A study published in Science, however, argues that this is the wrong approach.
This research, by Jan Medlock and Alison Galvani, indicates that the greatest public health benefit from vaccines is the “herd immunity” effect, which helps to break a disease’s transmission chain. Rather than focusing on those most at-risk for a disease, better results may be had by vaccinating those most likely to spread the disease. In this case, that would mean school-age children (who have highly concentrated social contact at school) and their parents (in particular, adults between 30 and 40 years old). Under our current system, these groups are at the bottom of the priority list.
Drs. Medlock and Galvani used the infamous Spanish Flu epidemic of 1918 and the epidemic of 1957 as models for the ways influenza spreads in humans. They evaluated the potential benefits of different vaccination programs in a number of ways. Their calculations took into account the infections and deaths that could be averted, as well as more sophisticated methods that considered economic valuations, including the costs of the programs vs. productivity gains.
In their study, no matter which epidemic pattern was analyzed, and no matter which way they measured the benefits of vaccination, the most desirable approach was always the same. Rather than vaccinate infants and the elderly, the best results against influenza was to vaccinate young people and their parents. Also, the researchers calculated that by using such an approach, the number of vaccinations in the U.S. could be lowered from a typical 85 million doses to just over 60 million.
For swine flu (N1H1), the CDC is again recommending that the most susceptible individuals should be targeted for vaccination. With that disease, however, the at-risk population is happily much closer to the population of “spreaders” – those who are most likely to pass the disease along through high levels of social contact.
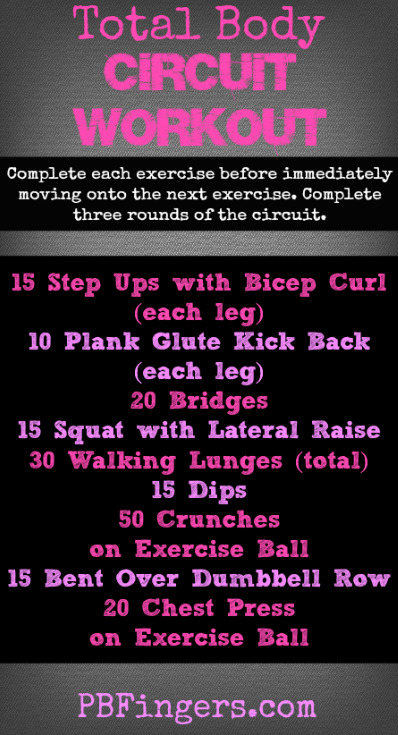
With or without vaccination, washing your hands, covering your mouth when coughing or sneezing, and avoiding close contact with those who are already sick will substantially reduce the risk of spreading the infection. Give your immune system a fighting chance by eating well, getting moderate exercise and a good night’s sleep. Smoking hits your immune system hard, so find a way to stop. Chinese herbal medications can really help to dampen the effects of flu, and keep it from getting strongly established in your system. Check with a board certified herbalist and/or your medical doctor if you are already taking medications or have complicating health issues.